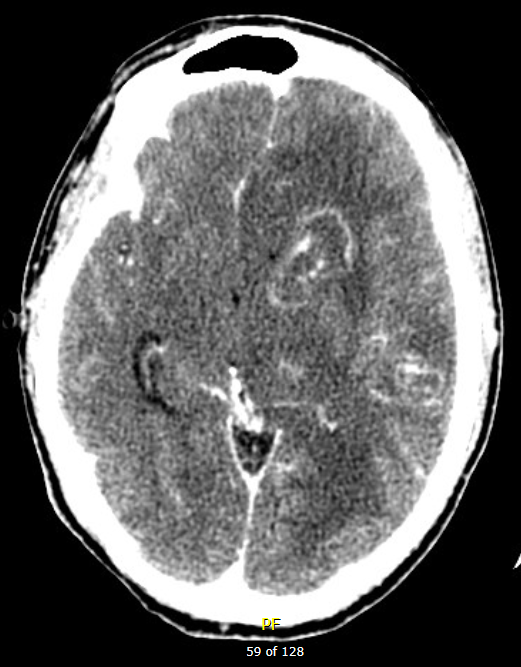
39M from DR, h/o AIDS (CD4 = 40, VL 250k) not on HAART, p/w AMS, also have decreased ambulation/appetite/speaking/ambulation for 2 wks Vitals: 98.3/55/18 BP: 100/60
What is the differential diagnosis ?
expand
What to do for this patient ?
expandIf patient cannot take Sulfadiazine, Alterative: Clindamycin + Pyrimethamine + Leukovorin
or: IV Trimethoprim-sulfamethoxazole (TMP-SMX)
Work-up: Anti-toxoplasma IgG, absent of IgG make diagnosis unlikely, but can’t rule out(IgM usually absent, and IgG titer is NOT helpful); CSF PCR has high specificity (96-100%), but variable sensitivity (50-98%)
Follow-up: If no response to treatment within 10-14 days, should consider alternative diagnosis AND consider brain biopsy
Duration of treatment: usually 6 weeks.
From NEJM Teaching Topics | February 23, 2012
Q. What neoplastic processes are part of the differential diagnosis of a peripherally enhancing brain lesion?
The differential diagnosis of a peripherally enhancing brain lesion should always include the following neoplastic processes: metastatic tumors, primary glial tumors, and primary lymphoma of the central nervous system. Although tumor metastases may cause a solitary peripherally enhancing lesion, such lesions are more commonly multifocal. High-grade glioma may cause a solitary, rim-enhancing lesion as the relatively rapid tumor growth outstrips the blood supply, leading to central necrosis. However, both anaplastic astrocytoma and glioblastoma are more typically heterogeneously enhancing and often cross the midline. Primary lymphoma of the central nervous system, usually diffuse large B-cell lymphoma, may occur in otherwise healthy persons. Alternatively, it may occur as part of advanced infection with human immunodeficiency virus (HIV), in which case it is characteristically associated with detectable Epstein–Barr virus (EBV) DNA in the cerebrospinal fluid. It is usually homogeneously enhancing, although cases involving patients who are HIV positive may be heterogeneous or peripherally enhancing.
Q. What is the typical presentation of CNS toxoplasmosis?
A. Toxoplasma is a protozoon that rarely causes serious illness in normal hosts. In patients with advanced HIV infection, however, it is the most common cause of focal brain mass lesions. Patients with toxoplasma infection typically present subacutely with headache, fever, changes in mental status, and focal neurologic deficits. Imaging studies of the brain reveal characteristic rim-enhancing lesions that are usually multifocal but may be solitary in up to 30% of cases. Lesions are typically less than 4 cm in diameter. Serologic testing for toxoplasma IgG would be helpful, since this test has high sensitivity for toxoplasma exposure. However, antibodies may be lost in patients with profound immunosuppression, and seroprevalence is higher in Europe than in the United States. These lesions characteristically improve rapidly with appropriate treatment. Therefore, if the clinical scenario allows observation, a trial of specific antimicrobial agents may be both therapeutic and diagnostic.